PTSD
What It Actually Is:
PTSD is what happens when your brain gets stuck in survival mode after something terrible. Your nervous system learned that the world isn't safe, and now it won't let you forget that lesson. The alarm system that'ssupposed to protect you from danger keeps firing even when the danger is long gone.
This isn't drama. It's not being "too sensitive." Your brain recorded a threat, encoded it deep, and now it replays that recording whether you want it to or not. Nightmares, flashbacks, that constant feeling like something bad is about to happen. Your body remembers what your mind has tried to move past.
What This Looks Like in Real Life:
You're fine until you're not. A smell, a sound, a certain look on someone's face, and suddenly you're back there. Or you're never really fine, just operating with this low-level dread humming in the background all the time, exhausted from being on alert 24/7.
You avoid things. Places, people, conversations, anything that might trigger the memory. Your world gets smaller because it feels safer to stay away from anything that could set you off. Sleep becomes a battleground. You either can't fall asleep because your brain won't quiet down, or you wake up in a sweat from dreams that feel more real than your actual life.
You might feel numb. Disconnected from people you care about. Like you're watching your life from behind glass. Or you might feel everything too intensely, irritable and reactive in ways that don't match the situation. Sometimes both, swinging between shutdown and explosion.
How This Wrecks Things:
PTSD doesn't stay contained. It leaks into everything. Relationships suffer because you're either emotionally unavailable or so reactive that people start walking on eggshells around you. Work gets harder because concentration is shot and you're running on fumes. You might start drinking or using something to take the edge off, which creates its own set of problems.
The isolation is brutal. People who haven't been through it don't understand, and explaining feels impossible. So you stop trying. You pull back. And loneliness makes everything worse.
Depression and anxiety often show up alongside PTSD. Sometimes it's hard to tell where one ends and the other begins.
The Numbers:
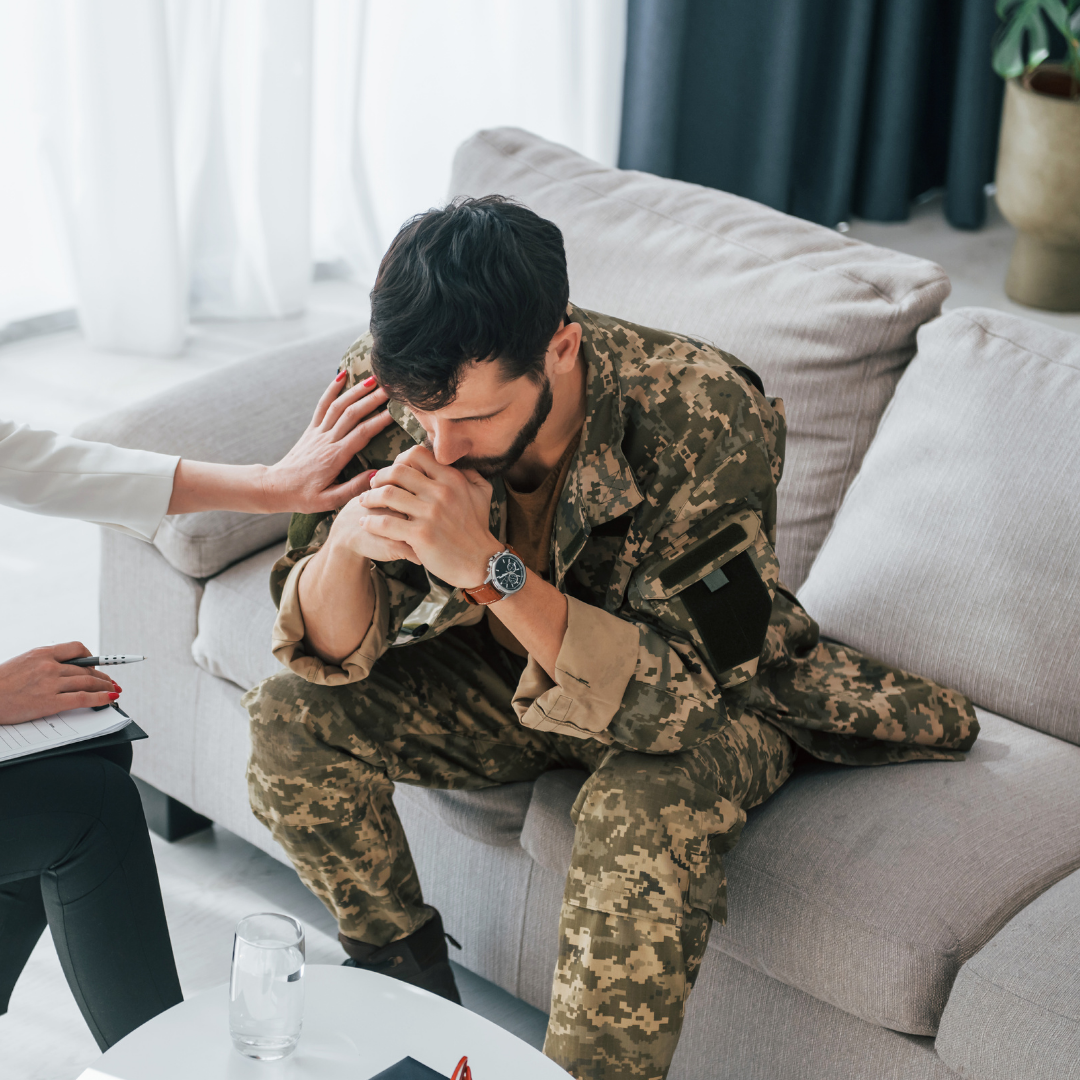
About 8% of Americans will deal with PTSD at some point. Women are diagnosed about twice as often as men, though that might have more to do with reporting than actual rates. Men aren't exactly encouraged to admit they're struggling with trauma. A lot of people are walking around with undiagnosed PTSD because they think trauma only counts if you were in combat or survived something "bad enough."
There's no threshold for bad enough. If it changed how your brain operates, it counts.
What Actually Works:
Trauma-focused therapies have the best evidence. EMDR (Eye Movement Desensitization and Reprocessing) sounds weird but it works. It helps your brain reprocess the traumatic memory so it stops hijacking your present. Trauma-focused CBT is another solid option. These approaches actually address the stuck memory rather than just managing symptoms.
Medication can help stabilize things while you do the harder work. SSRIs can reduce hyperarousal and improve sleep. Prazosin specifically helps with trauma nightmares. We use medication as a tool to make the therapeutic work possible, not as a way to avoid it.
How We Do This:
We offer both in-person and telehealth appointments across Washington and Oregon. Trauma work requires trust, and we don't rush that. You need to feel safe before you can process what happened.
Here's what we won't do: We won't treat you like you're fragile. Trauma is real, and what happened to you matters. But you're not broken beyond repair, and you're not defined by the worst thing that ever happened to you. Our approach is about helping you process what happened so you can move forward, not about wallowing in it forever.
The goal isn't to forget. It's to remember without being controlled by the memory.
How Often You'll Come In:
Trauma work typically starts with weekly sessions. That frequency helps build momentum and keeps the process moving. We need to establish trust, stabilize symptoms, and then do the actual processing work. As things improve, we can spread out visits. But this isn't a quick fix. Real trauma treatment takes time, and rushing it doesn't work.